Introduction
Nosocomial infections can be defined as an infection
developed within a person during a stay in a hospital or any other healthcare
facility.
To be precise, any infection developed in a person while
receiving medical support in a health care setting, which was not present or
was not in the incubation period prior to the admission of the person in the
health care setting, is called nosocomial infection. To be a
nosocomial infection, the disease must be developed only after at least 48 of
admission to/visiting a healthcare facility.
It is also called ‘Hospital Acquired Infection (HAI)’
or ‘Healthcare Associated Infection (HCAI).’
The pathogens causing such infections are acquired during
the process of receiving healthcare facilities in facilities like hospitals,
nursing homes, clinics, diagnostic centers, rehabilitation centers, or any
other clinical centers. The infection can develop and be noticed during the
period of stay within such centers or may also be developed after
discharge.
The pathogens can be transmitted from any factors of the
hospital environment (like air, water, bedding, building, wastes, etc.),
hospital staff, medical devices, other patients, or any other objects. The
pathogen may be the normal flora of the patient itself. During a hospital stay,
if the immune system is compromised, the normal flora (opportunistic
pathogens within or on the patient’s body) develops the infection. Such
infections are also called nosocomial infections. If the
incubation periods of such pathogens are shorter than the duration of hospital
stay, the disease is observed during the period of stay within the hospital.
However, if the incubation period is longer than the duration of the patient’s
stay in the hospital, the disease is developed after the discharge of the
patient.
Types of Nosocomial Infections
The US Center for Disease Control and Prevention (CDC)
categorizes nosocomial infections, broadly into the following 4 most frequent
types:
Central Line-associated Bloodstream Infection (CLABSI)
These are the bloodstream infections developed in patients
with central venous catheters (catheters inserted in veins for administration
of intravenous medications). It is common in patients in ICUs and is one of the
major causes of HAI-associated morbidity and mortality globally; with about 12
to 25% mortality rate in the USA in 2020.
Catheter-associated Urinary Tract Infection (CAUTI)
These are urinary tract infections (infections developed in
the urinary tract) in persons with indwelling urinary catheters. It is the most
common form of HAIs and is the prime cause of secondary bloodstream infections.
A major case of complicated UTI cases is associated with urinary
catheterization.
Surgical Site Infections (SSI)
These are the infections developed in or around the site
where surgery was done within 30 days of surgery. The infection can be
superficial or limited to the epidermal layer (Superficial SSI), deep beneath
the incision area in muscle (Deep Incisional SSI), or infecting inner organs
(Space SSI).
Ventilator-associated Pneumonia (VAP)
Pneumonia is the second most common nosocomial infection
after UTI seen in patients with critical illness and the associated mortality
rate may be up to 50%. If a patient receiving mechanical ventilator support
develops pneumonia after 48 hours of being incubated, then pneumonia can be
defined as ventilator-associated pneumonia.
Besides, there are other types of nosocomial infections,
viz.:
Gastroenteritis/Gastrointestinal Infections
Gastrointestinal infections seen in patients after at least
48 hours of admission, during their stay in the healthcare facility, or within
3 days of being discharged from the healthcare facility can be defined as
nosocomial gastroenteritis.
Nosocomial Skin Infection
Infection of the skin due to exposure to pathogenic
microorganisms in a healthcare facility is called nosocomial skin
infection. After a long hospital stay or use of antimicrobials and/or
other medications making the immune system weak, the normal skin flora of the
patients begins to develop several forms of skin infections like rashes,
ulcers, cellulitis, folliculitis, pyogenic and non-pyogenic wounds, etc. The
most common causative is Staphylococcus spp.; either normal flora
or Staph transmitted from other patients or most commonly healthcare
workers.
Non-catheter-associated Bloodstream Infections and Urinary Tract Infections
These are bloodstream infections and urinary tract
infections seen in hospitalized (including recently discharged) patients without
any catheterization.
Non-ventilator-associated Pneumonia (NVAP)and other
Respiratory Tract Infections
In hospitalized patients without ventilator support, several
forms of respiratory tract infections are seen; all these RTIs fall under this
category. While VAP is associated primarily with aerobes, the
non-ventilator-associated RTIs are caused by aerobes, anaerobes, as well as
respiratory viruses.
Nosocomial infections can also be classified on the basis of
associated pathogenic microorganisms into bacterial, fungal, and viral
nosocomial infections.
Risk Factors
The common risk factors associated with the development of
nosocomial infections are listed below:
- Immunocompromisation
Patients with immune-compromised conditions due to any
disease or administration of medical products are likely to develop nosocomial
infections more often than patients with healthy/functional immune
systems.
- Invasive
Medical Procedures including Catheterization
Invasive medical procedures like surgery, catheterization,
angioplasty, medical device insertion, thrombectomy, coronary stenting, etc.
increase the risk of the introduction of pathogens directly into the dermal or
muscular region escaping the primary layer of defense, the skin. This will make
the patent more prone to the development of infections. Similarly, medical
devices allow the route of administration of pathogens and also allow for
biofilm formation; hence, increasing the chance of infection.
- Prolonged
Use of Antimicrobials
Prolonged use of antimicrobials will inhibit normal flora,
allowing colonization of other pathogenic organisms from the environment.
Similarly, some antimicrobials also tend to weaken the immune system increasing
the chance of infection.
- Prolonged
Hospitalization
Prolonged hospitalization increases the risk of exposure to
pathogens increasing the chance of acquiring nosocomial infection.
- Use
of Contaminated Medical Devices
Medical devices like thermometers, pulse-oximeter,
sphygmomanometers, etc. are used for multiple patients without sterilization.
This will also increase the risk of transmission of pathogens.
- Contact
with other Patients and Career Medical Personals
Pathogens from other patients and medical personnel can be
transmitted to susceptible patients visiting healthcare settings.
- Chronic
Diseases
Chronic diseases like HIV, COPD, cancer, etc. make a person
more susceptible to nosocomial infection.
- Age
Age is also a major factor influencing the chance of
acquiring HCAIs. Elderly people and neonates are more susceptible than children
and adults.
Epidemiology of Nosocomial Infections
These types of infections are reported globally and can
occur in any healthcare setting. In general, about 10% of admitted persons are
reported to be infected with a type of hospital-acquired infection. Among the
hospital-admitted patients, patients in intensive care units (ICU), burn units,
and surgical or post-surgical wards suffer from HAIs.
The prevalence rate is a little higher in developing
countries than in developed countries. In high-income (developed) countries
about 7 in 100 i.e. 7% and 15 in 100 i.e. 15% of
patients admitted to acute health care services are infected with at least one
nosocomial infection. Among HAI-acquired patients, about 10% will die from the
infection; hence, it is one of the major causes of mortality and morbidity in
healthcare settings. The date is, however, different in different
regions/countries. There is no regular study done on this topic in every
country, so the exact rate of prevalence is difficult to determine. The
US CDC reports that about 3.2% of hospitalized patients in the USA develop at
least one nosocomial infection.
Common Pathogens Responsible for Nosocomial Infections
Bacterial infections are the most common types of nosocomial
infections followed by fungal and viral infections. Parasitic infections are
rarely encountered; hence they contribute a negligible portion of nosocomial
infections.
Bacterial Pathogens
They are the most common types of microorganisms causing
HCAIs. Both opportunistic and true pathogenic bacteria cause HCAIs. Some common
bacterial pathogens associated with nosocomial infections are:
|
Gram-Positive Bacteria |
Gram-Negative Bacteria |
|
Staphylococcus aureus (Methicillin
Resistant Staphylococcus aureus (MRSA), |
Enterobacterales (E. coli, Klebsiella spp., Proteus
mirabilis, Enterobacter spp., Salmonella spp., etc.) |
Fungal Pathogens
Fungi account for most of the HCAIs after bacteria. They
mainly infect severely immunocompromised patients, patients with severe
granulocytopenia, and ventilated patients. Some common fungal pathogens
associated with nosocomial infections are:
- Candida spp. (Candida albicans, fluconazole
resistant C. krusei, C. glabrata)
- Aspergillus spp. (A. fumigatus, A. flavus)
- Mucorales (Mucor spp.)
- Fusarium spp.
- Pneumocystis jirovecii
- Scedosporium spp.
- Malassezia spp.
- Acremonium spp.
Viral Pathogens
Several viruses are responsible for a minor portion of
nosocomial infections. Some common viruses causing nosocomial infections are:
- Noroviruses
- Rotaviruses
- Influenza viruses
- Respiratory syncytial virus
- Herpes Simplex Virus
- Hepatitis B and C virus
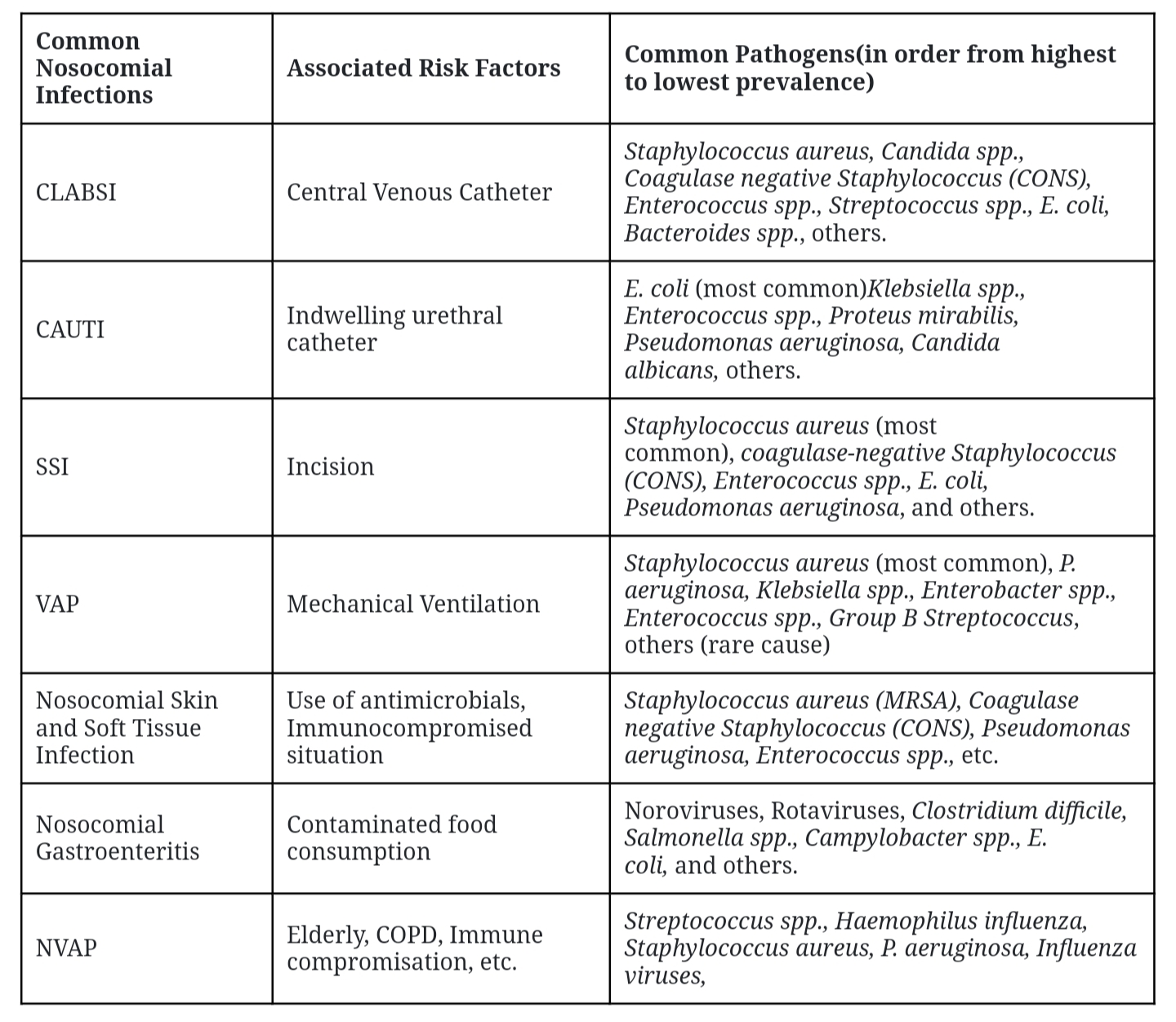
Common Nosocomial Infections and Associated Risk Factors and Pathogens
Common Source/Reservoir of Pathogens Associated with
Nosocomial Infections
- Healthcare
setting staff (including both clinical and non-clinical personnel)
- Environmental
aspects like surface, water, food, air, patient room, bathroom, basin,
bedding, door knobs, medical devices, etc.
- Patients
(normal flora of patients themselves or microbiome from other
patients)
- Visiting
members of patients
- Hospital
wastes
- Animals
like pests, insects, and others in the healthcare facility
Transmission of Nosocomial Infections
- Contact
transmission: Direct contact with patients or healthcare workers or
contact with contaminated surfaces and equipment.
- Droplet
transmission: From infectious respiratory droplets produced during
coughing, sneezing, speaking, etc., or during medical procedures.
- Airborne
transmission: Infectious agents can transmit over long distances via
contaminated air.
- Fecal-oral
transmission: Fecal-contaminated food and water ingestion can also
transmit nosocomial infections.
- Vector
transmission: Vectors such as insects and rodents can spread pathogens
in healthcare settings.
- Vehicle
Transmission: The vehicle includes food, water, medical devices,
syringes, PPEs, body fluid-contaminated materials, etc.
Impact of Nosocomial Infection on Patients
- Increased
morbidity and mortality rate
HCAIs make the case worse and/or cause secondary infections
and increase the morbidity and mortality rate of patients.
- Prolonged
hospital stay
The nosocomial infections will increase the severity of the
case demanding prolonged hospital stays and more medicines for treatment.
- Chance
of antimicrobial-resistant infections
Nosocomial infections are often caused by
antimicrobial-resistant species transmitted from hospital settings.
Hospitalized patients are often administered antibiotics which can induce the
development of antimicrobial resistance in patient-associated microorganisms.
- The
increased cost of treatment
Increased case morbidity and antimicrobial-resistant
infections demand prolonged hospital stays and more medicines for treatment
which will increase the cost of treatment.
Antibiotic Resistance and Nosocomial Infections
Healthcare settings are the primary source of origin and
dissemination of antimicrobial-resistant species because they are the place
where antimicrobials are mainly used and pathogens from different sources are
accumulated. Many pathogens causing HCAIs are found to be
antimicrobial-resistant strains and the cases of antimicrobial-resistant
associated HCAIs are increasing rapidly across the globe.
ESKAPE is
a group of multi-drug resistant pathogenic bacteria, mostly responsible for
nosocomial infections. This group includes 6 pathogens, viz. Enterococcus
faecium (Vancomycin Resistant Enterococcus faecium), Staphylococcus aureus
(MRSA and VRSA), Klebsiella pneumoniae (Carbapenem resistant Klebsiella
pneumoniae (CRKP)), Acinetobacter baumannii (Carbapenem resistant Acinetobacter
baumannii (CRAB)), Pseudomonas aeruginosa (Carbapenem resistant Pseudomonas
aeruginosa (CRPA)), and Enterobacter spp. (Pan-drug resistant Enterobacter
spp.). Besides, Beta-lactamase producing Enterobacterales,
drug-resistant Candida spp., and other fungal pathogens,
drug-resistant Streptococcus spp. are also serious threats to
nosocomial infections.
These AMR pathogens increase the chance of HCAIs, case
severity, prolonged hospital stay, increased cost of treatment, and higher
mortality.
Prevention, Control, and Management of Nosocomial Infections
For the prevention, control, and management of nosocomial
infections, the following measures should be adopted.
The practice of good hand hygiene– Healthcare workers
should practice good hand hygiene like washing with soap and water, use of
gloves, or use of hand sanitizers before and after visiting a patient.
Similarly, the family person visiting or taking care of the patients must
follow hand hygiene. This will reduce the transmission of pathogens from
healthcare workers to patients.
Proper and regular sanitization of hospital setting–
Healthcare settings including patient rooms, beddings, equipment, surfaces,
etc. must be regularly disinfected and cleaned.
Regular monitoring and surveillance of the
hospital environment for any potential pathogens is necessary. The data from
such a program will allow the infection control department to make effective
plans to prevent and control nosocomial infections.
Patient isolation– Patients with infectious diseases
and patients with higher susceptibility to infections must be isolated.
Antimicrobial stewardship can help to reduce the
probability of emergence/development and spread of AMR pathogens.
Use of PPE (personal protective equipment)– PPE like
globes, masks, goggles, aprons, body suits, etc. is very important to prevent
the transmission of pathogens in healthcare facilities. Healthcare workers must
use PPE so that they can prevent acquiring and transmitting pathogens from one
patient to another. Patients must also use general PPE like masks and gloves
during their stay and visit to healthcare facilities.
Immunization can play a very important role in
developing immunity against possible HCAIs.
Educating healthcare workers/staff regarding HCAIs,
their mode of transmission, and methods to prevent such diseases can be a very
effective method to prevent and control the spread of HCAIs in a healthcare
facility.
Minimize the hospital visit and hospital stay duration if
possible, because prolonged hospital stay will increase the risk of being
infected with HCAIs.
Proper management of hospital wastes and proper
pest control is also very important to prevent the emergence and
spread of infection in hospitals.
Ensuring proper implication of strategies and plans to prevent and control HCAIs is also very important.