Introduction
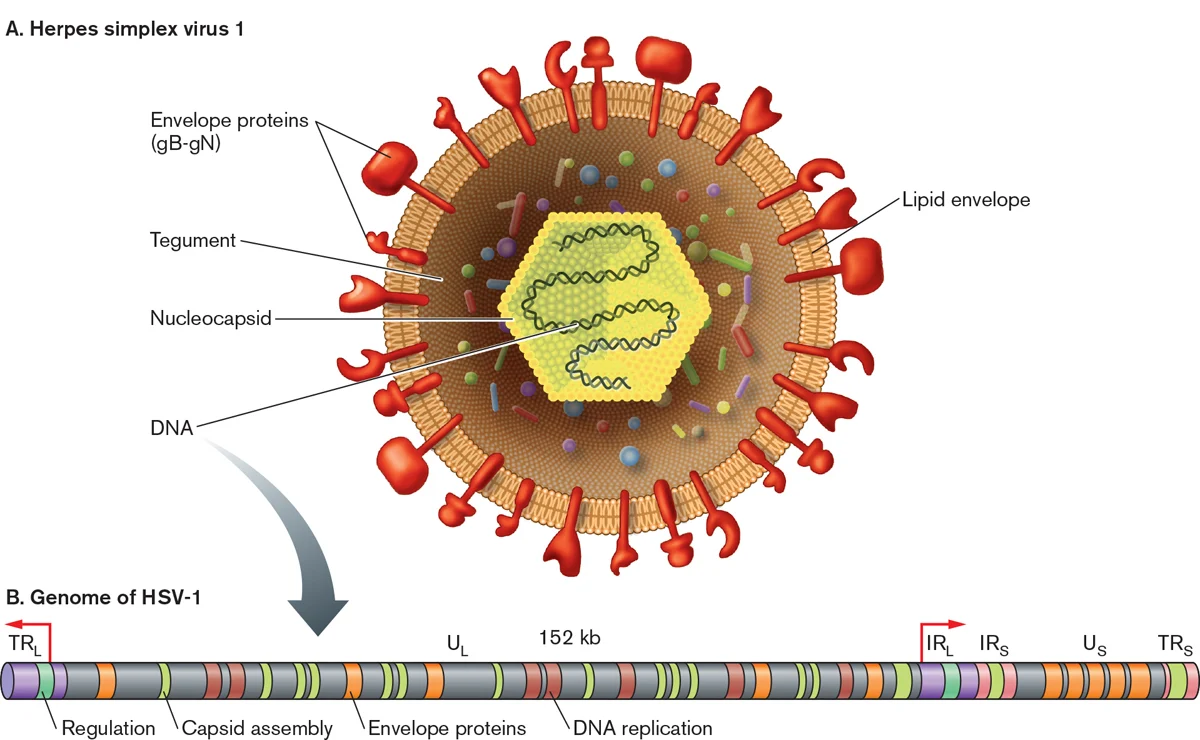
- Herpesviruses
are large (150-200 nm size), spherical in shape with icosahedral symmetry.
- The
icosahedral protein capsid with average diameter 100 nm consists of 162
hollow hexagonal and pentagonal capsomeres with an electron-dense core
containing the double stranded DNA genome with 125-240 kbp nucleotides
together forming the nucleocapsid.
- The
nucleocapsid is surrounded by an envelope which is lipoprotein in nature.
- Lipid part is derived from the nuclear
membrane of the infected host cell.
- Projecting
from the trilaminar lipid host-derived envelope are spikes of viral
glycoproteins, 8nm long, which bind to specific host receptor and mediate
virus entry.
- HSV
encodes for at least 11 glycoproteins that serve as (a) viral
attachment proteins (gB, gC, gD, gH), (b) fusion proteins (gB), (c)
structural proteins, (d) immune escape proteins (gE, and gI), and (e)
other fractions.
- In
mature virus particles, outside the capsid is an amorphous proteinaceous
layer, the tegument, surrounded by a lipid envelope derived from host cell
membranes.
- The tegument consist of enzymes such as VP16 which is responsible for subverting cellular proteins and enzymes to involve in viral nucleic acid replication and VHS (Virion Host Shut off ) protein which shut off the host cell protein synthesis in the cytoplasm.
Genome of Herpes simplex virus 1 (HSV-1)
- The
virus contains double-stranded DNA genome and is linear with molecular
weight of 125–240 kbp.
- The
herpesvirus genome is large comprising of 60- 120 genes and encodes at
least 100 different proteins.
- Of
these, more than 35 polypeptides are involved in the structure of the
virus particle and at least 10 are part of the viral envelope.
- Herpesviruses encode an array of virus-specific enzymes involved in nucleic acid metabolism, DNA synthesis, gene expression, and protein regulation (DNA polymerase, helicase-primase, thymidine kinase, transcription factors, protein kinases).
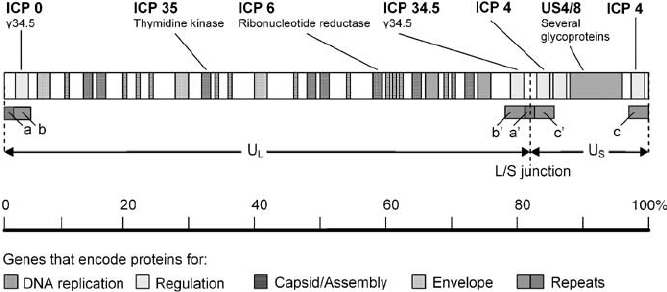
- A
striking feature of herpesvirus DNAs is their sequence arrangement
possessing terminal and internal repeated sequences.
- On
the basis of sequence arrangement it is divided into 6 types – A,B,C,D,E
and F.
- Type
E genome is found in Herpes Simplex virus.
- The
termini of class E consist of two elements.
- The
terminal sequences (ab and ca) are inserted in an inverted orientation
separating the unique sequences into long (Ul) and short (Us) domains.
Epidemiology of Herpes simplex virus 1 (HSV-1)
- Herpes
simplex viruses are worldwide in distribution, equally between the sexes,
and without seasonal variation.
- HSV-1
infection is more common than HSV-2 infection with 65% of persons in the
United States having antibodies to HSV-1.
- The
epidemiology in Europe is similar, with at least half of the population
seropositive for HSV-1.
- In
the developing world, HSV-1 is almost universal, and usually acquired from
intimate contact with family in early childhood.
Transmission of Herpes simplex virus 1 (HSV-1)
- HSV-1
infection is transmitted orally through saliva.
- It
is usually transmitted by oral contact, such as by kissing or by sharing
of the toothbrushes or other saliva-contaminated items.
- The
HSV infection can also occur following mouth-to-skin contact, with the
virus entering through minor abrasions in the skin.
- Autoinoculation
may also cause infection of the eye.
Replication of Herpes simplex virus 1 (HSV-1)
- Invasion of cells by HSV1 requires binding of the envelope gC (glyco-protein-C) and/or gB to Heparan sulfate receptors, engagement by gD of one of several co-receptors including HveA (Herpes virus entry mediator A, also known as HVEM, Herpes Virus Entry Mediators), fusion of the viral envelope with the cell plasma membrane and delivery of the viral capsid into the cell cytoplasm.
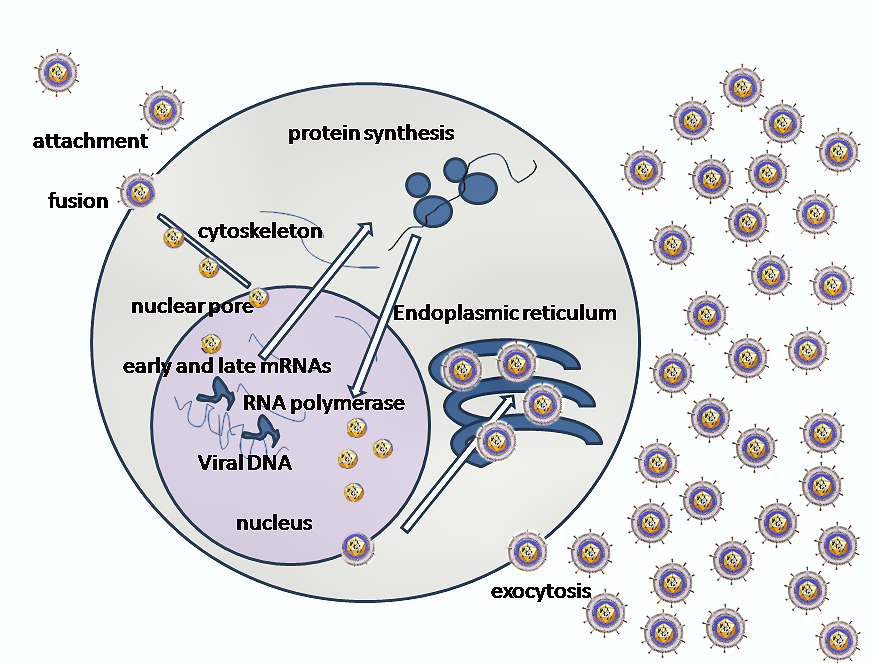
- Along
with the capsid viral proteins VHS and VP16 are also released in the
cytoplasm.
- The
incoming viral capsids are subsequently propelled to nucleopore for entry
in the nucleus where it gets disintegrated and only DNA is released into
the nucleus.
- The
viral genome is uncoated for viral transcription and replication in the
nucleoplasm.
- There
are two main phases of transcription–early, which takes place prior to
genome replication, and late, which takes place upon replicated genomes in
virus replication compartments formed in the infected cell nucleus.
- Three
distinct classes of mRNAs are made: Alpha, Beta, and Gamma which are
regulated in a coordinated, cascade fashion.
- The
Alpha or IE (Immediate-early) genes contain the major transcriptional
regulatory proteins and their production is required for the transcription
of the Beta and Gamma gene classes.
- The
Beta proteins include the enzymes that are required for replication of the
viral genome: a DNA polymerase, a single-strand DNA-binding protein, a
primosome or helicase-primase, an origin-binding protein, and a set of
enzymes involved in DNA repair and in deoxynucleotide metabolism.
- Viral
DNA synthesis begins shortly after the appearance of the Beta proteins and
the temporal program of viral gene expression ends with the appearance of
the Gamma or late proteins, which constitute the structural proteins of
the virus.
- The
linear 153Kb pair genome circularizes shortly after infection of
susceptible host cells and then enters a rolling circle mode of DNA
replication generating branched concatameric DNA, which is then cleaved to
release linear ds DNA.
- Viral
transcription and DNA replication occurs in the nucleus; the particle
assembles and exits from epithelial cells in the skin causing a primary
infection.
- The
virion acquires its envelope by budding through the nuclear membrane.
Pathogenesis of Herpes simplex virus 1 (HSV-1)
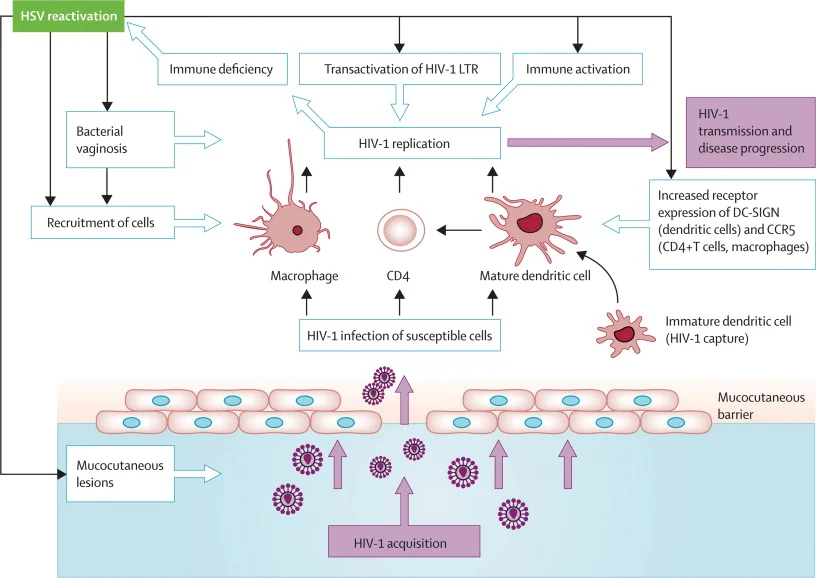
- HSV-1
is spread by kissing or exchanging saliva.
- The
virus is usually acquired in childhood or during sexual activity, either
through oral–oral or oral–genital contact.
- HSV-1
infects epithelial cells and infection begins with the attachment of virus
particles to susceptible cells.
- Virions
interact with specific cell-surface receptors through glycoproteins that
project from the viral envelope.
- The
typical lesion produced by HSV is the vesicle, a ballooning degeneration
of intra-epithelial cells, which contains infectious fluid.
- The
base of the vesicle contains multinucleate cells (Tzanck cells) and
infected nuclei contain eosinophilic inclusion bodies.
- The roof of the vesicle breaks down and an ulcer forms.
- This
happens rapidly on mucous membranes and non-keratinizing epithelia; on the
skin, the ulcer crusts over, forming a scab, and then heals.
- Natural
killer (NK) cells play a significant role in early defenses by recognizing
and destroying HSV-infected cells.
- HSV
shows three unique biological properties: neurovirulence, latency, and
reactivation.
- After
the infection at the local site of incoluation virus then invades the
local nerve ending; and is transported by retrograde axonal flow to the
dorsal root ganglia, where it replicates further, and then undergoes
latency.
- Primary
HSV infections are usually mild; in fact most are asymptomatic.
- Latency
means non replicating state and undergoes in trigeminal ganglia.
- HSV
does not replicate in latent stage except for a small RNA, called
micro-RNA (encoded by a latency- associated viral gene) which maintains
the latent infection and prevents cell death.
- Reactivation
processes are still not clearly understood.
- It
is suggested that HSV DNA passes along the nerve axon back to the nerve
ending where infection of epithelial cells may occur.
- Not
all reactivation will result in a visible lesion; there may be
asymptomatic shedding of virus only detectable by culture or DNA detection
methods.
- The
factors influencing the development of recrudescent lesions are not yet
clearly identified.
- An
increase of CD8+ T suppressor lymphocyte activity is common at the time of
recurrences.
- Some
mediators (e.g. prostaglandins), and a temporary decrease in immune
effector cell function, particularly delayed hypersensitivity, may enhance
spread of HSV.
- Certainly,
the known triggers for recurrences are accompanied by a local increase in
prostaglandin levels, and depression of cell-mediated immunity predisposes
to herpes recurrence.
- It
occurs naturally, and can be induced by a variety of stimuli such as
ultraviolet light (sunlight), fever, trauma and stress.
- The
interval between the stimulus and the appearance of a clinically obvious
lesion is 2–5 days; this has been demonstrated regularly in patients
undergoing neurological interference with their trigeminal ganglion, a
common site of herpes latency.
Clinical manifestations of Herpes simplex virus 1 (HSV-1)
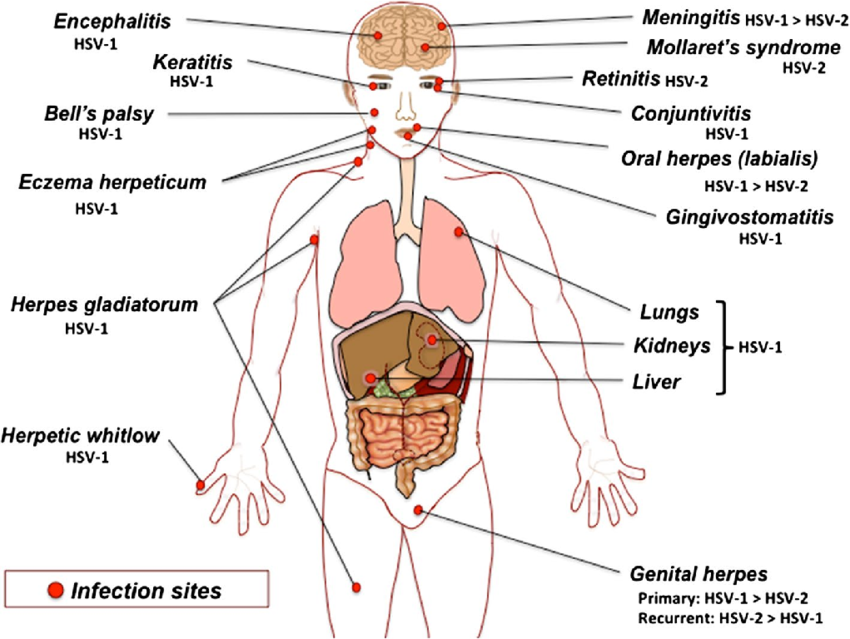
A. Oropharyneal disease
- Primary
HSV-1 infections are usually asymptomatic.
- Symptomatic
disease occurs most frequently in small children (1–5 years of age) and
involves the buccal and gingival mucosa of the mouth.
- Vesicular
lesions ulcerate rapidly and are present in the front of the mouth and on
the tongue (stomatitis).
- Gingivitis
(swollen, tender gums) is the most striking and common lesion.
- Primary
infections in adults commonly cause pharyngitis and tonsillitis.
- Vesicles
may also develop on the lips and skin around the mouth (herpetic
dermatitis), and cervical lymphadenopathy can occur.
- Recurrent
disease is characterized by a cluster of vesicles most commonly localized
at the border of the lip.
- Lesions
progress through the pustular and crusting stages, and healing without
scarring usually completes in 8–10 days.
- The
lesions may recur, repeatedly and at various intervals, in the same
location.
- The
frequency of recurrences varies widely among individuals.
B. Keratoconjunctivitis
- HSV
infection of the eye may be periorbital together with conjunctivitis, or
keratoconjunctivitis associated with corneal ulceration or as vesicles on
the eyelids.
- With
recurrent keratitis, there may be progressive involvement of the corneal
stroma, with permanent opacification and blindness.
C. Skin infections
- Localized
lesions caused by HSV-1 may occur in abrasions that become contaminated
with the virus (traumatic herpes).
- These
lesions are seen on the fingers of dentists and hospital personnel called
as herpetic whitlow but other sites may be involved, on the bodies of
wrestlers called herpes gladiatorum as a result of direct skin to skin
contact.
D. Eczema herpeticum
- Cutaneous
infections are often severe and life threatening when they occur in
individuals with disorders of the skin, such as eczema or burns, that
permit extensive local viral replication and spread called as eczema
herpeticum or Kaposi’s varicelliform eruption.
- Extensive
ulceration results in protein loss and dehydration, and viraemia can lead
to disseminated disease with severe, even fatal consequences.
E. Meningitis/ encephalitis
- HSV-1
infections are considered the most common cause of sporadic, fatal encephalitis
in the United States.
- The
disease carries a high mortality rate, and those who survive often have
residual neurologic defects.
- Direct
infection from the nasal mucosa along the olfactory tract is one of the
possibility, but the most likely route is central spread from the
trigeminal ganglia.
F. Genital herpes
- The
prominent cause of genital herpes is HSV-2, however some clinical episodes
of genital herpes are caused by HSV-1.
- Primary
genital herpes infections can be severe, with illness lasting about 3
weeks.
- Genital
herpes is characterized by vesiculo ulcerative lesions of the penis of the
male or of the cervix, vulva, vagina, and perineum of the female.
- The
sign and symptoms include pain associated with fever, malaise and dysuria.
G. Neonatal herpes
- HSV
infection of the newborn may be acquired in utero, during birth, or after
birth.
- The
mother is the most common source of infection in all cases.
- Neonatal
herpes can be acquired postnatally by exposure to either HSV-1 or HSV-2.
- The
most common route of infection for HSV to be transmitted to a newborn
during birth is by contact with herpetic lesions in the birth canal.
- To
avoid infection, delivery by cesarean section has been used in pregnant
women with genital herpes lesions.
Laboratory Diagnosis of Herpes simplex virus 1 (HSV-1)
Specimens: vesicle swab, skin swab, vesicle
fluid, corneal scrapings, skin scrapings, oral swab, blood, tissue, CSF
Culture
- Inoculation
of tissue cultures is used for viral isolation.
- HSV
is easy to cultivate, and cytopathic effects usually occur in only 2–3
days.
- Virus
can rapidly grow in cell cultures of fibroblasts and epithelial types
where the virus produces characteristics grounding and ballooning of cell.
- The
agent is then identified by neutralization test or immunofluorescence
staining with specific antiserum.
Cytopathology
- Cytopathology
involves the detection of multinucleated giant cells in scrapings obtained
from the base of vesicle by staining with Giemsa or Wright’s stain,
commonly called as Tzanck smear preparation.
- Demonstration
of typical giant cells or cow dry type A intranuclear inclusion bodies in
the stained smear is diagnostic of HSV infection.
Antigen detection
- The
antigen can be detected in vesicle fluid, tissue smear and biopsy by
direct fluorescent antigen detection and direct enzyme immunoassay.
Antibody detection
- Antibodies
appear in 4-7 days after the infection and peak in 2-4 weeks.
- Primary
infection can be detected by determining the presence of IgM or the rising
titre of IgG by ELISA, IFT and Complement fixation test.
- Serologic
assays based on the type-specific antigens, glycoprotein G, can
differentiate between HSV-1 and HSV-2.
Molecular Diagnosis
- Polymerase
chain reaction (PCR) is the most sensitive test for detecting HSV DNA and
can be used to differentiate between HSV-1 and HSV-2.
Treatment of Herpes simplex virus 1 (HSV-1)
- Acyclovir
has a better therapeutic ratio and proven efficacy.
- Acyclovir,
a nucleoside analog, is monophosphorylated by the HSV thymidine kinase and
is then converted to the triphosphate form by cellular kinases.
- The
acyclovir triphosphate is efficiently incorporated into viral DNA by the
HSV polymerase, where it then prevents chain elongation.
- Besides
acyclovir, valacyclovir, and vidarabine are also used which inhibit DNA
synthesis.






![LATEX TEST FOR RHEUMATOID ARTHRITIS [RHEUMATOID FACTOR]](https://examtube.in/public/assets/images/blog/LNKhD-rheumatoid-factor.jpg)