Structure of Polio Virus
- Poliovirus
is a member of a family of viruses called the Picornaviridae.
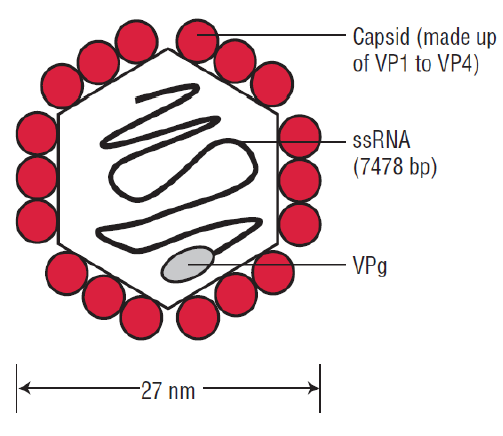
- Virions
are spherical in shape with a diameter of about 27nm.
- The
particles are simple in that they are composed of a protein shell
surrounding the naked RNA genome.
- The
genome is monopartite, linear ssRNA(+) genome of 7.2-8.5 kb,
polyadenylated, composed of a single ORF encoding a polyprotein.
- The
capsids are composed of four structural proteins: VP1, VP2, VP3, and VP4.
- The
basic building block of the picornavirus capsid is the protomer, which
contains one copy each of VP1, VP2, VP3, and VP4.
- The
shell is formed by VP1 to VP3, and VP4 lies on its inner surface.
- The
virus particles lack a lipid envelope, and their infectivity is
insensitive to organic solvents.
Genome of Polio Virus
- Polio
virus genome can be divided into three parts
- a
5′ noncoding region (NCR) that comprises approximately 10% of the genome,
is uncapped, and is covalently linked at the 5′ terminus to viral protein
VPg
- a
single open reading frame that appears to encode all of the viral
proteins, with regions designated as P1 for capsid proteins and P2 and P3
for nonstructural proteins
- a short 3′ NCR terminating in a polyA tail.
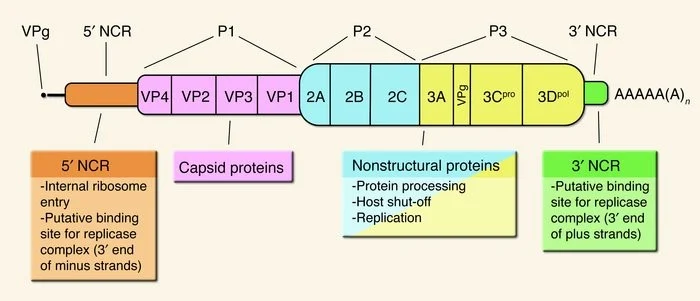
- The
genomes vary in length from 7,209 to 8,450 bases.
- The
5′-noncoding region contains the internal ribosome entry site (IRES), an
element that directs translation of the mRNA by internal ribosome binding.
- The
regions P1 contains four segments for structural proteins which make up
the capsid protein; 1A-VP4, 1B- VP2, 1C-VP3, 1D-VP1.
- P2
comprises of three non structural proteins; 2A, 2B, 2C which play a role
in viral replication.
- P3
makes up four non structural proteins
- 3A-
anchors the replication complex to cell membrane
- 3B-
it is VPg protein
- 3C-
it is cysteine protease that cleaves the protein from polypeptides
- 3D-
it is RNA dependent RNA Polymerase.
Epidemiology of Polio Virus
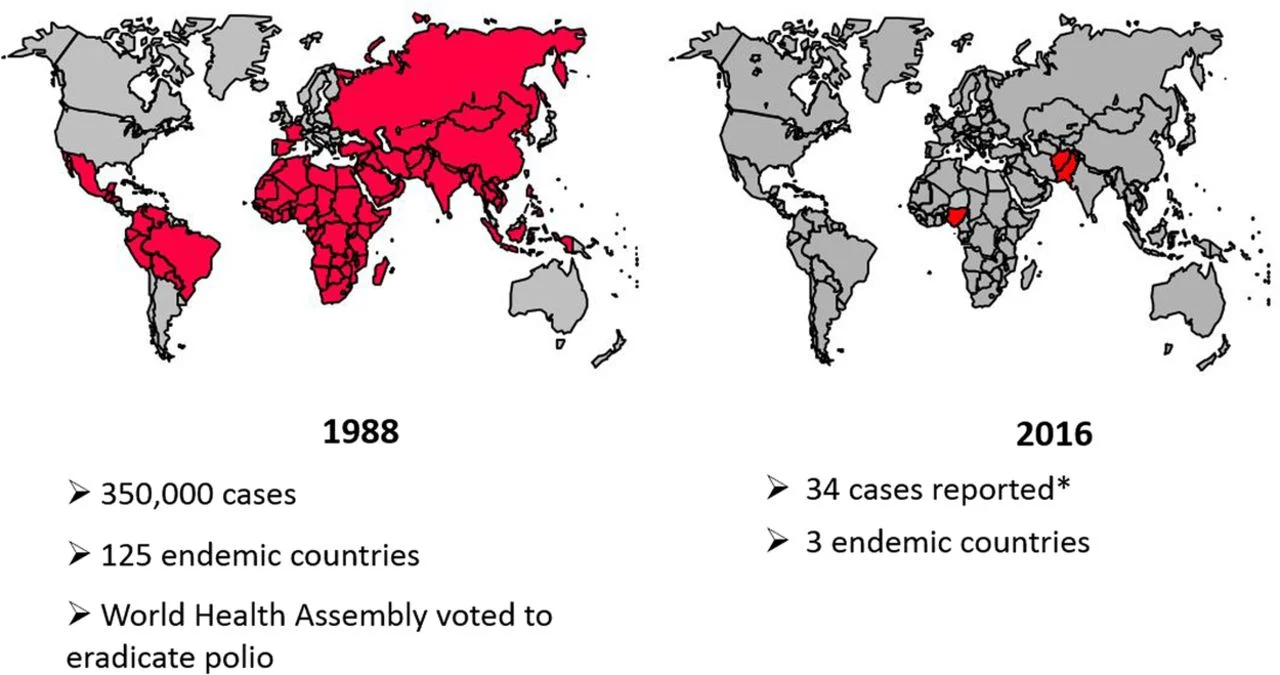
- Poliomyelitis
has had three epidemiologic phases: endemic, epidemic, and the vaccine
era.
- Before
global eradication efforts began, poliomyelitis occurred
worldwide—year-round in the tropics and during summer and fall in the
temperate zones.
- Winter
outbreaks were rare.
- The
disease occurs in all age groups, but children are usually more
susceptible than adults because of the acquired immunity of the adult
population.
- In
developing areas, where living conditions favor the wide dissemination of
virus, poliomyelitis is a disease of infancy and early childhood
(“infantile paralysis”).
- In
developed countries, before the advent of vaccination, the age
distribution shifted so that most patients were older than age 5 years,
and 25% were older than age 15 years.
- The
case fatality rate is variable and is highest in the oldest patients and
may reach from 5% to 10%.
- Before
the beginning of vaccination campaigns in the United States, there were
about 21,000 cases of paralytic poliomyelitis per year.
- Humans
are the only known reservoir of infection.
- In
temperate zones with high levels of hygiene, epidemics have been followed
by periods of little spread of virus until sufficient numbers of
susceptible children have grown up to provide a pool for transmission in
the area.
Replication of Polio Virus
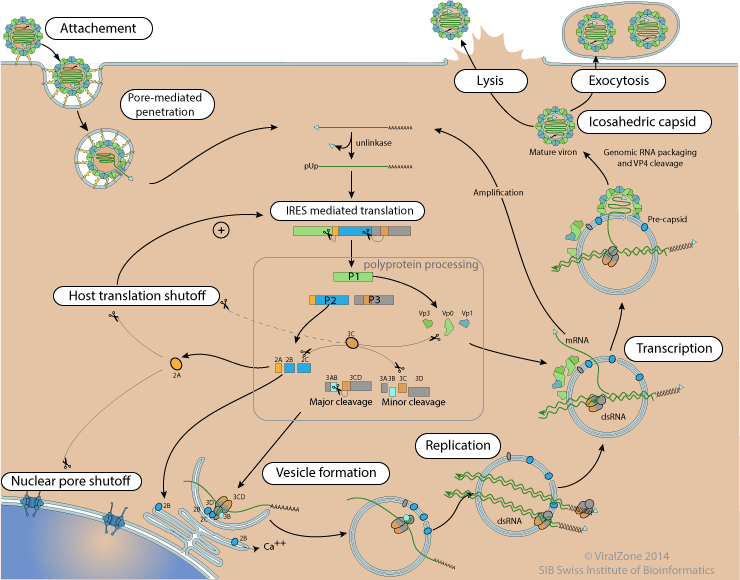
- Virus
binds to a cellular receptor and the genome is uncoated.
- VPg
is removed from the viral RNA, which is then translated.
- The
polyprotein is cleaved nascently to produce individual viral proteins.
- RNA
synthesis occurs on membrane vesicles.
- Viral
(+) strand RNA is copied by the viral RNA polymerase to form full-length
(–) strand RNAs, which are then copied to produce additional (+) strand
RNAs.
- Early
in infection, newly synthesized (+) strand RNA is translated to produce
additional viral proteins.
- Later
in infection, the (+) strands enter the morphogenetic pathway.
- Newly
synthesized virus particles are released from the cell by lysis.
Pathogenesis of Polio Virus
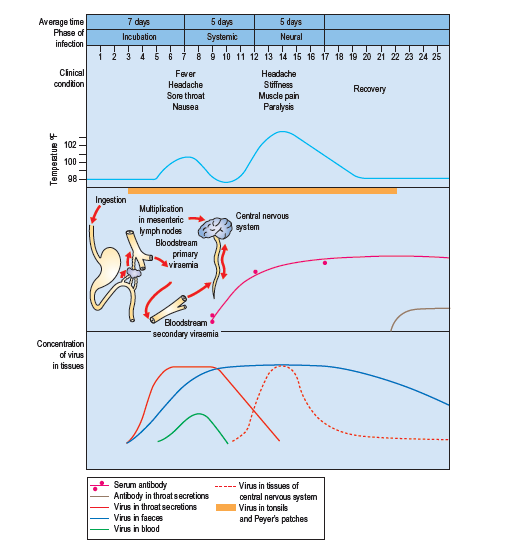
- The
mouth is the portal of entry for the virus, transmitted by fecal oral
route on ingestion of contaminated water.
- Virus
initially multiply in the oropharynx and gastrointestinal mucosa.
- The
virus is regularly present in the throat and in the stools before the
onset of illness.
- Virions
are resistant to acidity of stomach and to lytic activities of the
protease and other enzymes of the intestinal tract and bile.
- On
entering the body, the virus infects and multiplies in the tonsils and
Peyer’s patch of ileum.
- The
incubation period is 9-12 days.
- The
virus then spreads to regional lymph nodes and enters the blood causing
primary viremia.
- Antibodies
to the virus appear early in the disease, usually before paralysis occurs.
- The
antibodies are produced to prevent infection from spreading.
- On
continued infection and multiplication of virus in the ReticuloEndothelial
System (RES), it invades the blood stream causing secondary viremia.
- During
this period of viremia, the poliovirus crosses the blood brain barrier and
gain access to the brain.
- The
virus shows tissue tropism by specifically combining with neural cells.
- The
virus recognizes the receptor present on the anterior horn of spinal cord,
dorsal root ganglia and motor neurons.
- The
destruction of motor neurons leads to paralysis.
- The
virus also infects brain stem causing bulbar poliomyelitis.
Clinical Manifestations of Polio Virus
- The
earliest features associated with phase of viremia consist of fever,
malaise, headache, drowsiness, constipation, and sore throat and lasts for
1 to 5 days.
- Incubation
period is usually 10 days but may vary from 4 days to 4 weeks.
- Asymptomatic
illness
- It
is caused as a result of viral infection confined to the oropharynx and
the intestine.
- Abortive
poliomyelitis
- It
is minor illness occurring in approximately 5% of infected people.
- It
is febrile illness characterized by fever, headache, sore throat, loss of
appetite, vomiting, and abdominal pain.
- Neurological
symptoms are typically absent.
- Non
paralytic poliomyelitis
- Some
people who develop symptoms from the poliovirus contract a type of polio
that doesn’t lead to paralysis (abortive polio).
- This
usually causes the same mild, flu-like signs and symptoms typical of other
viral illnesses.
- Signs
and symptoms, which can last up to 10 days, include: Fever, sore throat,
headache, vomiting, fatigue, back pain or stiffness, neck pain or
stiffness, pain or stiffness in the arms or legs and muscle weakness or
tenderness.
- Paralytic
poliomyelitis
- Initial
signs and symptoms of paralytic polio, such as fever and headache, often
mimic those of non-paralytic polio.
- Within
a week, however, other signs and symptoms appear, including: Loss of
reflexes, severe muscle aches or weakness and loose and floppy limbs
(flaccid paralysis)
- Post
poliomyelitis syndrome
- Post-polio
syndrome is a cluster of disabling signs and symptoms that affect some
people years after having polio.
- Common
signs and symptoms include: Progressive muscle or joint weakness and pain,
fatigue, muscle wasting (atrophy), breathing or swallowing problems,
sleep-related breathing disorder; such as sleep apnea, and decreased
tolerance of cold temperatures.
- Bulbar
poliomyelitis
- This
is caused due to involvement of the cranial nerves, most commonly 9th,
10th, and 12th.
- This
condition tends to be more severe with involvement of the muscles of the
pharynx, vocal cords and respiration.
- The
condition may cause death in 75% of the patient.
Laboratory Diagnosis of Polio Virus
Specimen: stool, rectal swab, throat swab, CSF
(rare)
- Microscopy
- Virus
can be detected in stool specimens by direct electron microscopy or also
by immune electron microscopy.
- Although
virus is rarely demonstrated in CSF, microscopy of CSF demonstrates
predominantly lymphocytic pleocytosis.
- Virus
isolation
- Virus
may be recovered from pharyangeal aspirations and feces.
- Virus
isolation from feces and throat swab is carried out by cultivation on
monkey kidney, human amnion, HeLa cells, Hep-2, Buffalo green monkey
(BGM), MRC-5 and other cell cultures.
- Cytopathogenic
effects appear in 3–6 days.
- Cytopathic
effects include cell retraction, increased refractivity, cytoplasmic
granularity, and nuclear pyknosis.
- An
isolated virus is identified and typed by neutralization with specific
antiserum.
- Serodiagnosis
- Demonstration
of fourfold increase of antibody titer in the serum sample collected at
the time of acute illness and time of convalescence.
- Neutralization
test and complement fixation test is carried out to demonstrate antibodies
presence.
- Molecular
diagnosis
- Virus
can also be identified more rapidly by polymerase chain reaction (PCR)
assays.
Treatment of Polio Virus
- No
antiviral treatments are available for the treatment of poliomyelitis.
Prevention and Control of Polio Virus
- Provision
of clean water, improved hygienic practices and sanitation are important
for reducing the risk of transmission in endemic countries.
- Immunization
is the cornerstone of polio eradication and both live-virus and
killed-virus vaccines are available.
- Formalin-inactivated
vaccine (Salk) is prepared from virus grown in monkey kidney cultures.
- Killed-virus
vaccine induces humoral antibodies but does not induce local intestinal
immunity so that virus is still able to multiply in the gut.
- Live
attenuated vaccine (Sabin) is grown in primary monkey or human diploid
cell cultures and delivered orally.
- The
live polio vaccine infects, multiplies, and immunizes the host against
virulent strains.
- The
vaccine produces not only immunoglobulin M (IgM) and IgG antibodies in the
blood but also secretory IgA antibodies in the intestine, enabling mucosal
immunity.
- Both
killed-virus and live-virus vaccines induce antibodies and protect the CNS
from subsequent invasion by wild virus.
- Oral
polio vaccine has been the vaccine used predominantly in the past in
global campaigns and is still used in endemic areas.
- It
has the advantages of inducing both humoral and intestinal immunity and of
being cheap and easy to administer.
- However,
the gut develops a far greater degree of resistance after administration
of live-virus vaccine indicating it as a potential limiting factor of
interference for oral vaccine.
- The
disadvantage is the small risk of vaccine associated paralytic
poliomyelitis (VAPP), which occurs in about 4 out of every 1,000,000
vaccinated children and unvaccinated contacts.
- Inactivated
poliovirus vaccine is injected intramuscularly and does not carry any risk
of VAPP.
- The
disadvantage of inactivated vaccine is that it does not confer intestinal
immunity and is not effective for outbreak control and is more expensive
and requires better trained staff for deliverance.
- European countries have gradually shifted from OPV to IPV over the last decades and today all EU Member States use IPV in their childhood immunization programmes.