What is Chromoblastomycosis (Chromomycosis)?
Chromoblastomycosis that is also known as
chromomycosis is a chronic fungal infection of the skin and the subcutaneous
tissue, caused by different groups of dematiaceous fungi.
- It
is one of the most encountered subcutaneous fungal infections besides
sporotrichosis and mycetoma.
- Dermateciuos
fungi are fungi that are pigmented, producing brown pigmentations.
- The
disease is associated with slow-growing, warty plaques, cauliflower-like
lesions which may ulcerate.
- It
majorly affects immunocompromised individuals with a weak immune system
which makes them liable to colonization and infection by these fungi.
- The
fungi have a form of traumatic implantations i.e inoculation of the fungi
is due to traumas such as wounds or abrasions of the skin, which exposes
the skin to the fungi infection.
- The
disease commonly affects male agricultural workers but few cases on
children’s infections have also been documented.
Causative agents of Chromoblastomycosis (Chromomycosis)
- Chromomycosis
is caused by dematiaceous fungi.
- Dermatiaceous
fungi are a large group of heterogenous molds known to cause a wide range
of skin infections including phaeohyphomycosis, chromoblastomycosis, and
eumycotic mycetoma.
- This
group of pathogenic fungi includes Fonsecaea pedrosoi, Phialophora
spp, Cladophialophora bantiana, Rhinocladiella, and Exophiala
spp, Mudurella spp, Scedosporium prolificans, Wangiella dermatitidis.
- The
most common etiologies of chromomycosis fungi are Cladosporium
carrionii, Phialophora verrucosa, and Fonsecaea pedrosoi and the
least common include Fonsacea compactum, Exophiala spinifera,
Rhinocladiella aquaspersa, Exophiala jeanselmei, and Wangiella
dermatitidis.
- They
are widely distributed in the environment, commonly found in soil, wood,
and dead decaying plant debris.
- They
are also common in tropical and subtropical climates.
- They
contain melanin of their cell walls which determines the color of the
spores.
- They
reproduce asexually by forming spores known as conidia.
- They form colonies in mycological agar which are typically brown to black in color.

Pathogenesis of Chromoblastomycosis (Chromomycosis)
- The
fungi gain entry into the skin from trauma from vegetative materials such
as thorns or splinters initiating a granulomatous response on the skin
- Mostly,
the fungal infection remains asymptomatic (oligosymptomatic) for several
years before it appears.
- The
moderate appearance of the disease is characterized by localized pain and
intensified itching which progresses to severe disease associated with
edema and secondary bacterial infection which may limit body motions and
activities.
- The
chronic disease shows manifestations of chronic lymphoedema and
development of ankylosis and non-invasive squamous cell carcinoma which
may lead to patient disablement.
General manifestations will also include:
- The
epidermis producing pseudoepitheliomatous hyperplasia, granuloma on the
dermis associated with epithelioid cells, and Langhans giant cells.
- Fungal
elements which are visualized as brown septate celled sclerotic bodies.
- Several
sets of sclerotic cella include medlar bodies, muriform bodies, copper
pennies.
- These
bodies are extruded trans-epidermally which are seen as black dots on the
surface lesions.
Risk factors of infection
- Immunocompromised
patients with skin abrasions such diabetics
- Patients
on medical therapies
- Wounded
and surgical patients
- Agricultural
workers who get skin scratching (abrasions) from plants
Virulence factors of dematiaceous fungi
- The
virulence of dematiaceous fungi is associated with the presence of melanin
in their cell walls, which confers a protective advantage by scavenging
free radicals and hypochlorite that are produced by phagocytic cells.
- The
melanin may also bind to hydrolytic enzymes, preventing the action of
phagocytic cells on the plasma membrane of the fungal cells.
- The
melanin gives color to the fungal spores and the fungal hyphae produced
during the germination and reproduction of these fungi. This gives the
fungi a pigmentation that produces colored skin lesions and skin
manifestations.
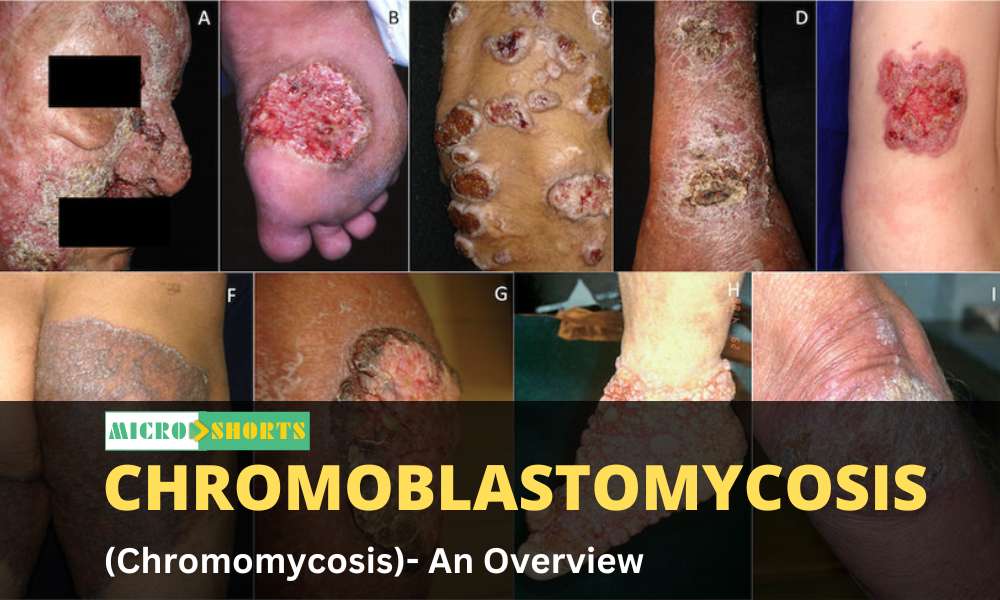
Clinical Features of Chromoblastomycosis (Chromomycosis)
Chromoblastomycosis is presented with:
- Small
firm red or grey bump.
- The
bump grows slowly about 2mm per year.
- A
dr warty nodule or plaque develops with centered
scarring.
- The
affected limb enlarges causing elephantiasis
- The
scarred lesion then forms new lesions around the scar allowing spread to
new sites with itchiness.
- Squamous
cell carcinoma may develop due to longterm infection of
chromoblastomycosis.
The lesions developed during chromoblastomycosis infections
include:
- Nodular
lesions are moderately elevated, fairly soft, with a dull to pink
violaceous growth with a smooth surface, verrucous, or scaly. They
gradually become tumorous with time.
- Tumoral
lesions are tumor-like masses, prominent, papillomatous, sometimes lobulated;
‘cauliflower-like’; covering the surface partially or entirely with
epidermal debris and crusts. they are more exuberant and occurs majorly in
lower extremities.
- Cicatricial
lesions are non-elevated with an enlarged peripheral extension and
atrophic scarring. They have centered healing. They have an annular,
arciform, or serpiginous outline and they can occur extensively in parts
of the body.
- Plaques
are slightly elevated lesions occurring in various sizes and shapes with
infiltration. They are reddish to violaceous in color with a scaly surface
and may have marked lines of cleavage. They are generally found on the
higher parts on the limbs.
- Verracuous
are outwardly hyperkeratosis lesions that are warty dry and are commonly
found along the border of the foot.
Diagnosis of Chromoblastomycosis (Chromomycosis)
Clinical Diagnosis
Clinical observation of lesions and differentiation from
other characteristic lesions formed by other microbial agents and fungal agents
as described above.
Laboratory Diagnosis
Specimen: Lesion exudates, skin scrapings, crusts,
aspirated debris, and tissue fragments
Direct examination and microscopy
- 20-40%
KOH wet mount to observe muriform (single or clustered) cells in clinical
samples which are 5 to 12 µm in diameter, round to polyhedral (chestnut)
in shape, thick-walled, dark pigmented, and having both transverse and
longitudinal cross-walls resembling a brick wall.
- Hematoxylin-eosin
staining for tissue samples for observation of the muriform cells.
- Calcofluor
white dye stain
Cultural Examination
- Use
of mycological and bacterial cultures to isolate pigmented fungal spores
which are examined by KOH wet mount for identification of muriform cells.
- However,
cultural methods are inadequate and unconventional therefore require to
follow up examination using staining and microscopic techniques.
Histological Examination
- Tissue
samples and biopsies for the identification of lesion particles such as
granulomatous tissue elements, and giant cells from lesions.
Molecular Identification of agents
- Duplex
PCR targeting the ribosomal DNA for Fonsecaea spp., and a
specific oligonucleotide primer for identification of C. carrionii
Immunological Examination
- This
can be used to identify the production of antibodies against the fungal
antigens such as ELISA assay using C. carrionii antigen
AgSPP.
Treatment of Chromoblastomycosis (Chromomycosis)
- Treatment
for Chromoblastomycosis includes physical therapeutic methods as well as
topical and systemic therapy with antifungal agents, which have been
documented to be effective.
- Physical
Therapeutics includes surgery, thermotherapy, laser therapy, and
photodynamic therapy (PDT) along with combined therapies of antifungal
drugs.
- Use
of antifungal agents such as itraconazole(ITZ), voriconazole (VCZ), PCZ,
and isavuconazole (ISA). Itraconazole is used as the first line of
treatment for CBM and Terbinafine is the second most frequently used
antifungal agent for the treatment of CBM.
- Combination
therapy with systemic antifungal drugs has been used in the salvage
therapy scenario for patients with invasive refractory mycoses such as a
combination of itraconazole with terbinafine.
- Combined
therapy may also include the use of antifungal agents along with physical
therapeutics such as surgeries.
- Adjuvant
therapy has also been used as a form of treatment which includes the use
of antifungal drugs with immunomodulant adjuvants in severe and refractory
cases of infection. Adjuvants such as Imiquimod, (1→3)-β-polyglucoside
have been used with itraconazole and terbinafine antifungals.
- BM
treatment must be monitored by clinical, mycological, and
histopathological criteria to ensure clearance of lesions and scars for
conclusively complete healing of the disease.
Antifungal Resistance of causative agents of chromoblastomycosis
- Chromoblastomycosis
is a chronic fungal infection that has shown resistance to normal
antifungal therapies such as fluconazole and amphotericin B, and therefore
the use of broad-spectrum therapies such as itraconazole and terbinafine
are used.
Prevention and Control of chromoblastomycosis
- Due
to a lack of vaccines specific for chromoblastomycosis, it advised that
the use of protective clothing such as gloves, shoes, and clothes to
reduce the risk of infection by ubiquitously dematiaceous fungi,
especially to the occupationally risky groups.