Structure of Influenza A Virus
- Influenza A virus falls under the family Orthomyxoviridae.
- Influenza A virus particles are usually spherical
and about 80- 120 nm in diameter.
- It is an enveloped virus and the envelope contains
two glycoproteins, hemagglutinin (HA) and neuraminidase (NA), the membrane
(M2) protein and is internally lined by the matrix (M1) protein.
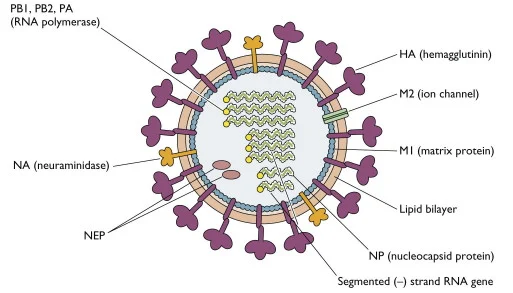
- The HA, so-called because the virus agglutinates
certain species of erythrocyte, is about 10 nm in length and consists of
trimers of identical glycoprotein subunits, each consisting of two
polypeptide chains, HA1 and HA2 joined by a linkage site that may be a
single basic amino acid, usually arginine, or a string of basic amino
acids.
- The Neuramindase (NA) on the other hand is tetramer
which facilitates release of virus particles from infected cell surfaces
during budding process and helps prevent self aggregation of virions by
removing sialic acid residues from viral gycloproteins via sialidase enzyme.
- They have a helical nucleocapsid comprising eight
segments of single-stranded RNA of negative sense.
- Influenza virus particles contain nine different
structural proteins.
- The nucleoprotein (NP) associates with the viral
RNA to form a ribonucleoprotein (RNP) structure 9 nm in diameter that
assumes a helical configuration and forms the viral nucleocapsid.
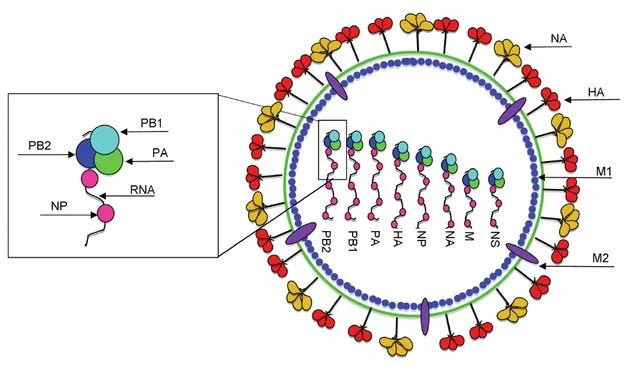
Figure: Structure of the
influenza A virus. The antibody response to the influenza A virus typically
targets the surface glycoproteins HA and NA, while the T-cell mediated response
typically targets the relatively conserved internal proteins including NP, M1,
and PB1. Source: DOI: 10.1615/CritRevImmunol.2013010019
- Three large proteins (PB2, PB1, and PA) are bound
to the viral RNP and are responsible for RNA transcription and
replication.
- The matrix (M1) protein, which forms a shell
underneath the viral lipid envelope, is important in particle
morphogenesis and is a major component of the virion.
- M2, on the other hand, makes membrane channel
protein and facilitate uncoating.
- The non structural protein NS is further divided
into two parts NS1 that inhibits cellular mRNA translation and NS2 which
is responsible for nuclear export of viral ribonuclear protein.
Genome of Influenza A Virus
- The genome of influenza A virus is segmented
ssRNA(-) linear genome, encapsidated by nucleoprotein (NP).
- It contains 8 segments coding for proteins.
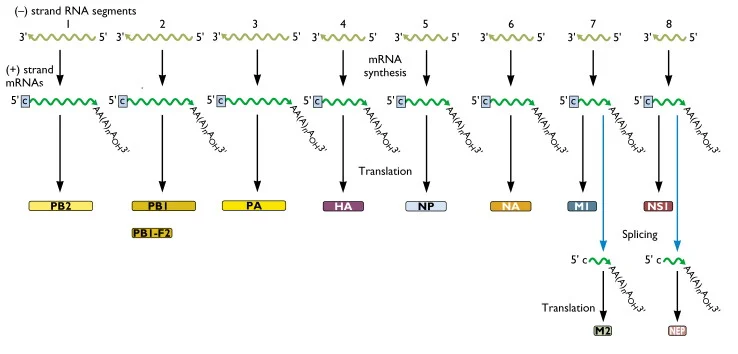
- Segments size range from 890 to 2,341nt and genomic
size is 13.5Kb.
- All the proteins are encoded on separate segments,
with the exception of the nonstructural proteins (NS1 and NS2) and the M1
and M2 proteins, which are transcribed from one segment each.
- The eight segments of genome comprise of PB2, PB1,
PA, HA, NP, NA, Matrix protein (M1 and M2), non structural proteins (NS1
and NS2).
- PB2, PB1 and PA are the polymerase proteins, have
transcription activity and convert the negative sense mRNA to
positive sense.
- Haemagglutination (HA) is responsible for viral
attachment, Nucleoprotein (NP) helps in making nucleocapsid and
Neuraminidase (NA) cleaves sialic acid and promotes viral spread.
- Matrix protein M1 makes inner lining of envelope
and promotes assesmbly and M2 make membrane channel protein facilitating
uncoating.
- Non structural protein, NS1 reduce interferon
reaction and inhibits RNA splicing.
- On the other hand, NS2 is required for the nuclear
export of viral RNP.
Epidemiology of Influenza A Virus
- Influenza A viruses are classified into subtypes
based on the antigenic difference of the major membrane glycoproteins HA
and NA.

Source: WHO, 2017
- Currently 18 HA subtypes and 11 NA subtypes are
found.
- The different combinations have been recovered from
birds, animal and humans.
- Four HA (H1, H2, H3, H5) and two NA (N1, N2)
subtypes have been recovered from humans.
- The virus infects multiple species including
humans, birds, swine, horses, seals, mink and whales with birds being the
primary reservoir.
- Influenza viruses occur worldwide and cause annual
outbreaks of variable intensity.
- It is estimated that annual epidemics of seasonal
influenza cause 3–5 million cases of severe illness and 250,000–500,000
deaths worldwide.
- The economic impact of influenza A outbreaks is
significant because of the morbidity associated with infections.
- Pandemics occurred in 1918, 1957 and 1968 with the
emergence of H1N1 Spanish influenza, H2N2 and H3N2 respectively, and most
recently in 2009, with the emergence of H1N1 from swine (H1N1 2009pdm)
into the human population.
- The great pandemic of 1918– 1919 was particularly
severe, killing 20–40 million people as it spread over a few years.
- Influenza A virus was first isolated from throat
washing of patient by Smith Andrews and Laidlaw in 1933.
- Major pandemics are associated with antigenic
shifts – when the viral HA or NA (or both) is changed.
- Antigenic shift results from the acquisition of a
complete new RNA segment 4 and/or 6, either as a result of reassortment or
infection of humans with an animal virus.
- Two influenza A subtypes have been circulating
concurrently, namely Influenza A H3N2 and Influenza A.
- Epidemics occurring regularly in winter months
between pandemics are associated with genetic drift in the HA antigen.
Replication in nucleus of Influenza A Virus
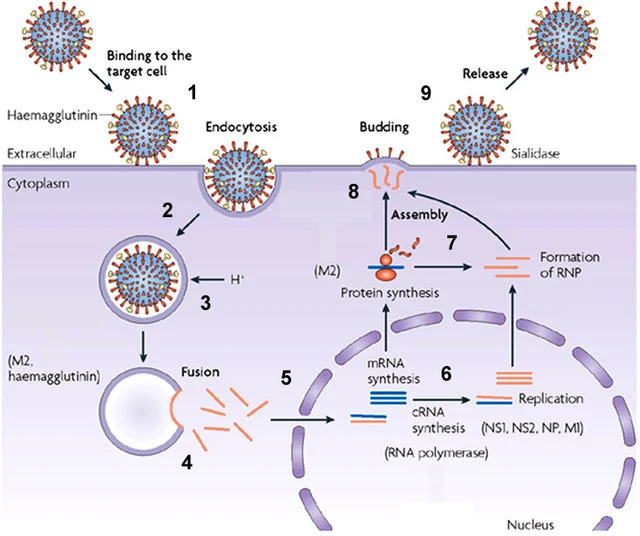
- Virus attaches to sialic acid receptor through HA
protein and is endocytosed by
clathrin mediated endocytosis into the host cell.
- After receptor-mediated endocytosis, the viral
ribonucleoprotein complexes are released into the cytoplasm and
transported to the nucleus, where replication and transcription take
place.
- Messenger RNAs are exported to the cytoplasm for
translation.
- Early viral proteins required for replication and
transcription, including nucleoprotein (NP) and a polymerase protein (PB),
are transported back to the nucleus.
- RNA polymerase activity of the PB1 protein
synthesizes positive single-stranded RNA (ssRNA) from genomic negative
single-stranded RNA (–ssRNA) molecules.
- These +ssRNA templates are copied by the RNA
polymerase activity of the PB1 protein.
- Some of these new genome segments serve as
templates for the synthesis of more viral mRNA.
- Viral mRNA molecules transcribed from some genome
segments encode structural proteins such as hemagglutinin (HA) and
neuraminidase (NA).
- These messages are translated by endoplasmic
reticulum-associated ribosomes and delivered to the cell membrane.
- Viral genome segments are packaged as progeny
virions and bud from the host cell.
Pathogenesis of Influenza A Virus
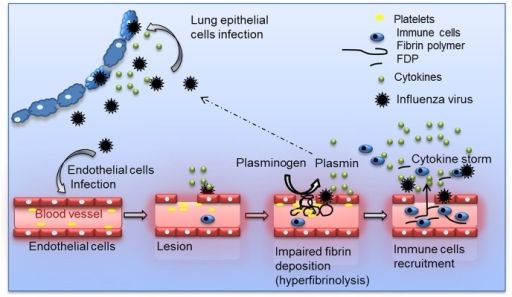
Figure: Schematic overview of the
proposed model for Plasminogen-mediated influenza virus pathogenesis. During
IAV infection, plasminogen is converted into plasmin. On the one hand, plasmin
cleaves and activates the viral hemagglutinin, promoting IAV replication for
some influenza strains. On the other hand, plasmin promotes inflammation via
fibrinolysis and increases permeability. Source: doi: 10.1371/journal.ppat.1003229.
- Influenza virus spreads from person to person by
airborne droplets or by contact with contaminated hands or surfaces.
- A person becomes infected when they inhale
microdroplets containing virus.
- The respiratory tract, upper and lower respiratory
tract have sialic acid to which HA portion of virus bind.
- A few cells of respiratory epithelium are infected
if deposited virus particles avoid removal by the cough reflex and escape
neutralization by preexisting specific immunoglobulin A (IgA) antibodies
or inactivation by nonspecific inhibitors inthe mucous secretions.
- The replication of virus takes place in nucleus and
progeny virions are soon produced and spread to adjacent cells.
- Viral NA lowers the viscosity of the mucous film in
the respiratory tract, laying bare the cellular surface receptors and
promoting the spread of virus-containing fluid to lower portions of the
tract.
- Within a short time, many cells in the respiratory
tract are infected and eventually killed.
- Additional flu like symptoms which include
sneezing, fever, chills, muscle ache, headache and fatigue occur.
- The incubation period from exposure to virus and
the onset of illness varies from 1 day to 4 days, depending on the size of
the viral dose and the immune status of the host.
- Viral shedding starts the day preceding onset of
symptoms, peaks within 24 hours, remains elevated for 1–2 days, and then
declines over the next 5 days.
- Interferon is detectable in respiratory secretions
about 1 day after viral shedding begins.
- If the virus spreads to the lower respiratory
tract, the infection can cause severe desquamation (shedding) of bronchial
or alveolar epithelium down to a single-cell basal layer or to the
basement membrane.
- Viral damage to the respiratory tract epithelium
lowers its resistance to secondary bacterial invaders especially
staphylococci, streptococci, and Haemophilus influenza.
- Influenza infection leads to an inflammatory cell
response of the mucosal membrane, which consists primarily of monocytes
and lymphocytes and few neutrophils.
- Submucosal edema is present.
- Lung tissue may reveal hyaline membrane disease,
alveolar emphysema, and necrosis of the alveolar walls.
- T-cell responses are important in aspects of
recovery and immunopathogenesis, but antibody, including vaccine-induced
antibody can prevent disease.
- Protection against reinfection is primarily
associated with the development of antibodies to HA, but antibodies to NA
are also protective.
- The antibody response is specific for each strain
of influenza, but the cell-mediated immune response is more general and is
capable of reacting to influenza strains of the same type.
Clinical manifestations of Influenza A Virus
- The typical incubation period for influenza is 1- 4
days (average: 2 days).
- Uncomplicated influenza illness is characterized by
the abrupt onset of constitutional and respiratory signs and symptoms
(e.g., fever, myalgia, headache, malaise, nonproductive cough, sore
throat, and rhinitis).
- Among children, otitis media, nausea, and vomiting
also are commonly reported with influenza illness.
- Uncomplicated influenza illness typically resolves
after 3—7 days for the majority of persons, although cough and malaise can
persist for >2 weeks.
- Influenza virus infections can cause primary
influenza, viral pneumonia; exacerbate underlying medical conditions
(e.g., pulmonary or cardiac disease); lead to secondary bacterial
pneumonia, sinusitis, or otitis media; or contribute to coinfections with
other viral or bacterial pathogens.
- Influenza virus infection also has been uncommonly associated with encephalopathy, transverse myelitis, myositis, myocarditis, pericarditis, and Reye’s

Complications of Influenza A Virus
- Tracheobronchitis and bronchiolitis– A small
proportion of patients develop more severe respiratory symptoms where
rales and rhonchi are heard but the chest is radiologically clear.
Pneumonia
- Primary viral pneumonia or a secondary bacterial
pneumonia may develop.
- Primary viral pneumonia is relatively uncommon,
but cases have been demonstrated in many influenza epidemics.
- Secondary bacterial pneumonia is more common than
primary viral pneumonia.
Secondary bacterial pneumonia
It usually occurs late in the course of disease,
after a period of improvement has been observed for the acute disease.
- The symptoms and signs are that of a typical
bacterial pneumonia.
- S. aureus is most commonly involved
although S. pneumoniae and H. influenzae may
be found.
- Infection of cells by influenza A requires
cleavage of the virus haemagglutinin by proteases, and some strains
of aureus produces such enzymes and hence promote
infection by damaging to the healthy respiratory epithelium.
Myositis and myoglobinuria– In addition to
myalgia, which is characteristic of acute influenza infection, clinical
myositis and myoglobinuria may occur.
Reye’s syndrome
Reye’s syndrome is characterized by encephalopathy
and fatty liver degeneration.
- The disease has a 50% mortality amongst
hospitalized cases and had been associated with several viruses; such as
influenza A and B, Coxsackie B5, echovirus, HSV, VZV, CMV and adenovirus.
Other complications
Influenza infections have been implicated in acute
viral encephalitis and Guillain-Barre syndrome.
- Influenza A was also associated with the cot death syndrome.

Laboratory diagnosis of Influenza A Virus
- Specimen– nasopharyngeal aspirate, throat
swab, nasal swab, tracheal aspirate, bronchoalveolar lavage (BAL), sputum
- Virus isolation
- Throat swabs, NPA and nasal washings may be used
for virus isolation.
- The specimen may be inoculated in embryonated eggs
or tissue culture.
- 10-12 day embryonated eggs are used for virus
isolation.
- The specimen is inoculated into the amniotic
cavity.
- The virus replicates in the cells of the amniotic
membrane and large quantities are released back into the amniotic fluid.
- After 2-3 days incubation, virus in the amniotic
fluid can be detected by adding aliquots of harvested amniotic fluid to
chick, guinea pig, or human erythrocytes.
- Pathological specimens can be inoculated on to
tissue cultures of kidney, chicks or a variety of other species, Rhesus monkey
cells being the most sensitive one.
- Although no CPE is produced, newly produced virus
can be recognized by haemadsorption using the cells in the tissue
culture, and haemagglutination using the culture medium which contains
free virus particles.
- Occasionally influenza A produce a CPE in MDCK
(Madin Darby Canine Kidney) cells.
- Influenza viruses isolated from embryonated eggs
or tissue culture can be identified by serological or molecular
methods.
Rapid diagnosis
- Cells from pathological specimens may be examined
for the presence of Influenza A antigen by Indirect Immunofluoresence
(IFA).
- Enzyme immunoassay (EIA) are available for
detection of viral antigen which are highly sensitive and specific.
- RT- PCR assays for the detection of influenza RNA
have also been developed.
Serology
Serological test is based on the demonstration of
a rise in antibody to the infecting virus.
- Complement fixation test (CFT) is the most common
method used using type specific soluble antigen, however the specificity
is low.
- Haemagglutination inhibition (HAI) test is more
specific in comparison to CFT. However, both the tests requires a 4-fold
or greater rise in antibody titre for detection.
- A more precise method for measuring antibody is by
Single Radial Haemolysis (SRH) and is more sensitive than CFT and HAI
test.
Treatment of Influenza A Virus
- Amantidine and Rimantidine are M2 ion channel
inhibitors, thus preventing the pH changes that precede the membrane
fusion step essential for nucleocapsid release.
- Zanamavir- potent inhibitor of neuraminidase and
administered by inhalation.
- Oseltamavir- inhibitor of neuraminidase and
administered orally.
Prevention of Influenza A Virus
- Vaccination is the most effective measure for
reducing the impact of influenza.
- In view of the changing antigenic characteristics of the virus, new vaccines are constantly required and should contain H and N components of prevalent strain.
Types of vaccine of Influenza A Virus
Killed vaccines
The vaccines are prepared from virus grown in
embryonated eggs and then chemically inactivated using formalin or beta
propiolactone.
- The quantity of HA is standardized in each vaccine
dose (~15 μg of antigen), but the quantity of NA is not standardized
because it is more labile under purification and storage conditions.
- The vaccine is conventionally formulated in
aqueous or saline suspension.
- The vaccine is administered by the subcutaneous or
intramuscular route.
Split virus vaccines
Split vaccines were prepared from inactivated
particles disrupted with detergents.
- These vaccines have been shown to induce fewer
side effects in the vaccinees and are just immunogenic as whole virus
vaccine.
Subunit virus vaccines
Subunit vaccines have been prepared by the
combination of HA and NA antigens.
- These are used in aqueous suspension or may be
absorbed to carriers such as alhydrogel.
Live attenuated vaccines
Normal methods for attenuation, such as repeated
passages and temperature adaptation require a long period to complete,
and probably too long for the vaccine to become available for
immunization against the current influenza strain.
- A trivalent live attenuated influenza vaccine is
administered as a single dose intranasal
- The trivalent vaccine consists of reassortant for
the HA and NA gene segments of the desired influenza strains, with a
master donor virus that is cold adapted to optimum growth at 25° C.
Control of Influenza A Virus
- Housing domestic poultry in shelters to avoid
contact with over-flying migrating birds.
- Eliminating wild bird markets.
- Segregating different species of birds in markets.
- Housing aquatic birds and domestic poultry
separately.
- Slaughtering domestic flocks infected with highly
pathogenic influenza A viruses.